|
White
Without Pressure (WWOP)
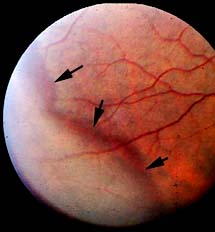
Retinal white without pressure (WWOP) is a
common retinal condition that is reported to
occur in up to 30% of the general population.
One study found WWOP in 2.5% of whites and 23%
of blacks. The incidence of WWOP increases with
age; it has been estimated to occur in
approximately 5% of eyes under age 20 years and
66% of eyes over age 70 years. Individuals with
increased axial length (high degrees of
nearsightedness) are more likely to develop WWOP.
Retinal WWOP appears as an area of the retina
that is translucent white to gray in color and
often is bounded posteriorly by a reddish-brown
line. This condition can mimic the appearance of
a shallow retinal detachment. WWOP may have
scalloped posterior borders (suggested to be a
sign of possible progression) and has been noted
to be migratory in nature; sequential fundus
examination reveals that the size, shape, and
location of WWOP may change over time. Areas of
WWOP frequently are associated with lattice
degeneration and snowflake degeneration. WWOP
may be circumferential and usually occurs
bilaterally. |
|
 |
|
WWOP usually is associated
with vitreous degeneration and posterior
vitreous detachment (PVD). Horseshoe retinal
tears or linear retinal tears can develop along
the posterior border of WWOP, and these tears
are associated with the traction of PVD.
In the management of a patient with WWOP, it is
important to consider factors that are
contributory to the development of retinal
breaks, such as the presence of lattice
degeneration, of scalloped borders (suggesting
progression over time), of shrinkage of the
vitreous (the jelly-like fluid filling the eye),
or of an elevated tractional membrane.
Patients with WWOP should be followed at 1- to
2-year intervals, depending on the presence of
other associated risk factors. The patient
should be reexamined every 6 months if the
posterior borders of the WWOP are scalloped and
there is extensive vitreous degeneration. As
patients reach their 40s and 50s, there is a
general increase in the risk of associated
retinal breaks and detachment because of
increased vitreous liquefaction and/ or vitreous
detachment (PVD). Caution should be exercised in
managing patients with high myopia because of
the association between increased axial length
and detachment. It is important to inform
patients about the signs and symptoms of retinal
detachment and watch carefully for breaks that
may develop at the posterior border of the
lesion.
The most important consideration in the
management of WWOP is the vitreoretinal traction
related to this condition. Vitreoretinal
traction is known to be associated with WWOP and
is strongly implicated in the genesis of retinal
tears and subsequent retinal detachments.
Patients with this condition should know that it
carries a low risk for complications but that it
is important to report symptoms or signs of
traction and breaks immediately. |